The ins and outs of cancer research: why a cure isn’t so simple.
Anneke Blackburn is a group leader at the John Curtain School of Medical Research at the Australian National University. Dr Blackburn specialises in cancer genetic research and has been involved in many projects, including ones based around breast cancer and blood cancer. She has received a number of grants to aid her research, but most recently on World Cancer Day, she was awarded a $65,000 grant from Cancer Council ACT. I met up with Dr Blackburn to discuss her research and how research grants help her to achieve these medical breakthroughs.

Q. What lead you into the cancer genetics area of research?
A. I started off doing science generally. It took me about ten years or so, maybe longer, before I actually got into cancer research. Before that I did a lot of biochemistry and pharmacology, I was always interested in drugs and drug metabolism and I joined a lab that had similar interests to me in terms of genetics but it was very much focused in cancer. I learnt a lot about cancer models there and focused on cancer genetics.
I realised trying to prevent cancer is actually really hard and it is difficult to get support for that. I still think that’s really important, but while we’re doing that we still need to treat people with cancer. In 2007 we started the work that is my interest now, which is trying to treat cancer through targeting cancer metabolism.
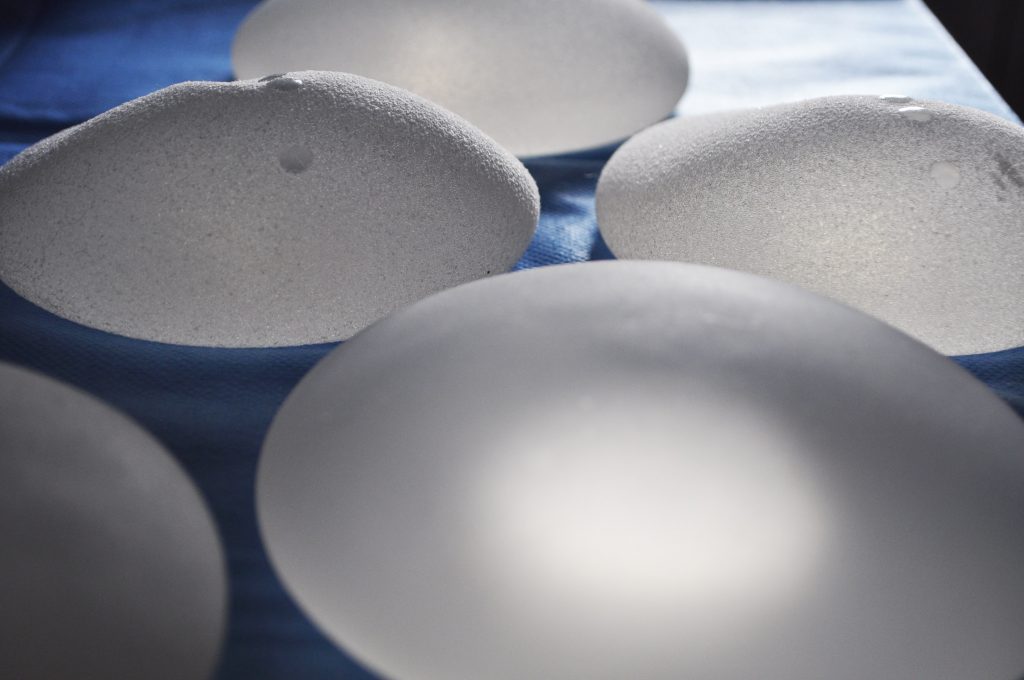
Previously I did work with breast cancer specifically on people more likely to get breast cancer due to genetic factors. Our work on treating cancer also started with breast cancer.
When it came to the point of actually looking for patients to test it in, it was haematologists that were most willing to participate and showed an interest with working the drug I was interested in. At that point, I made a bit of a switch into working on Myeloma, a blood cancer… So we worked on that and the drug we’re working with is called Dichloroacetate (DCA).
It is interesting and challenging because on its own it doesn’t tend to kill cancer cells but it can stop them growing and also make them more sensitive to the other drugs that are currently used in cancer treatment, which is where we started talking about a clinical trial. We first started in 2012 and we’re now just finishing writing the paper on that.
The primary goal of that trial, in the end, was just to see that it was safe to use this drug in patients. That’s the more recent work we’ve done on Myeloma with this drug but the first projects we did with this drug were on breast cancer. Again it was done mostly with breast cancer and it showed it would stop the cells from growing, stop the tumours from growing but on its own didn’t kill them until we combined it with other drugs that were capable of killing cancer cells
Attending residential for The Bridge Program, learning what is needed for translating drug research into real impact for patients. How to develop a winning pitch… pic.twitter.com/jdKFNiqUKz
— Anneke Blackburn (@AnnekeBlackburn) October 29, 2018
Q. What does it take to be allowed to start clinical trials?
A. You need to draw up a plan and an explanation of why you think it will work and you need to be really quite specific and that goes through an ethics committee with the hospital. They look at it and say well, yes, that’s a valid reason to test it on these people. The question is, is it fair on the patient to let them try this drug? When maybe they might be better off just doing the standard treatment.
The challenging thing now is working out what next to try on in patients. Because what it changes is the way that cells use their glucose and that change is very common over different cancer types.
The main thing is working out where the need is greatest, in particular, we need to work out which cancers are most likely to respond. We need to develop some sort of test that might help us identify the ones that look like this, the cancers that have these features, they’re the ones that are more likely to respond.
That’s part of the purpose behind the grant that we just got from the Cancer Council. We’re going to take lots and lots of different breast cancers, around 20 different breast cancers in the lab which have certain types of characteristics and see if we can work out a kind of signature of which ones are more likely to respond when we treat them with that drug.
Q. Are you able to use DCA in conjunction with standard treatments?
A. The expectation would be that we would be using it in conjunction with other medications. The difficulty is designing a trial and having patients similar enough that you could say, yes, it was better than the other one. It becomes quite difficult because you start getting different categories. So there are lots of different categories of breast cancer and then for each of those, there is a number of different treatment options they may have. You have to specify when you write a profile that you got a fairly homogeneous group of patients and you have to make sure there are enough of those patients out there.
Q. Is going for research grants competitive?
A. People spend a large portion of their year writing and preparing grants and experiments and projects. Which you know, is a good exercise to plan it all out, but frustrating if you don’t get it funded and you’ve spent all that time making a plan that you don’t actually get to do. So that’s one of the big frustrations.
There are some funds that come in through the University. A lot of research labs run off the university funds but in my positions, I’ve generally had to find my own salary of grants, so I’ve not had the financial support from the university for myself and this makes it harder to get things done sometimes.
Q. Does anyone but Cancer Council ACT do grants for you or have all the ones you’ve been given been from Cancer Council act?
A. I’ve had quite a few from the Cancer Council over the years working on this project. Some of the early ones were on breast cancer and then I had a large grant from them. One year they had a particularly large grant to give because someone had given a bequest to them so that was a much larger grant for three years and that got us going on the Myeloma rather than the breast cancer.
You can also get grants from the NHMRC, the National Health and Medical Research Council. That’s the standard place that researchers go when trying to get money for medical research. Typically, the system is changing at the moment, but usually, you get 3 year grants, but they’ll be $200,000 each and that’ll allow you to employ people.
The ones from the Cancer Council are really great for starting new projects. So they’re not really enough to employ somebody but you can use that to fund part of a person and also to provide lap support and lab materials and things you need for a student and to aid in their experiments. I’ve had some of the larger grants but not enough, so the smaller ones from the cancer council, they have been really, really important.



Be the first to comment!